Table of Contents
Discover how intermittent fasting naturally reduces inflammation by boosting your body’s own antioxidants. Stop frequent eating to start healing.
Every time you eat, insulin rises. Frequent snacking keeps this hormone elevated constantly, driving inflammatory processes throughout the body. Intermittent fasting flips this script by giving your system extended breaks from digestion. During these fasting windows, your body activates powerful internal antioxidant systems that combat oxidative damage. This mechanism makes fasting one of the most effective ways to reduce inflammation naturally without adding supplements or medications to your routine.
The problem with constant eating
Modern eating patterns look nothing like what humans evolved with. Our ancestors didn’t have refrigerators, drive-throughs or vending machines. They ate when food was available and went without when it wasn’t. Their bodies developed sophisticated mechanisms to thrive during both feeding and fasting states.
Today most people eat from the moment they wake until shortly before bed. Breakfast, mid-morning snack, lunch, afternoon snack, dinner, evening snack. Some nutrition advice even recommends six small meals daily to keep metabolism revved up. This guidance has proven disastrously wrong for metabolic and inflammatory health.
Every eating occasion triggers insulin release. Even protein and fat cause some insulin secretion, though far less than carbohydrates. When you eat constantly, insulin never returns to baseline. Chronically elevated insulin promotes inflammation through direct signaling pathways while simultaneously encouraging fat storage that produces its own inflammatory compounds.
The digestive process itself requires significant energy and generates metabolic byproducts. Your gut works hard breaking down food, absorbing nutrients and managing the trillions of bacteria involved in digestion. Constant feeding keeps this machinery running without rest, accumulating wear and promoting low-grade inflammation throughout the digestive tract.
What happens when you stop eating
Fascinating changes occur when you extend the gap between meals. These adaptations explain why fasting reduces inflammation so effectively.
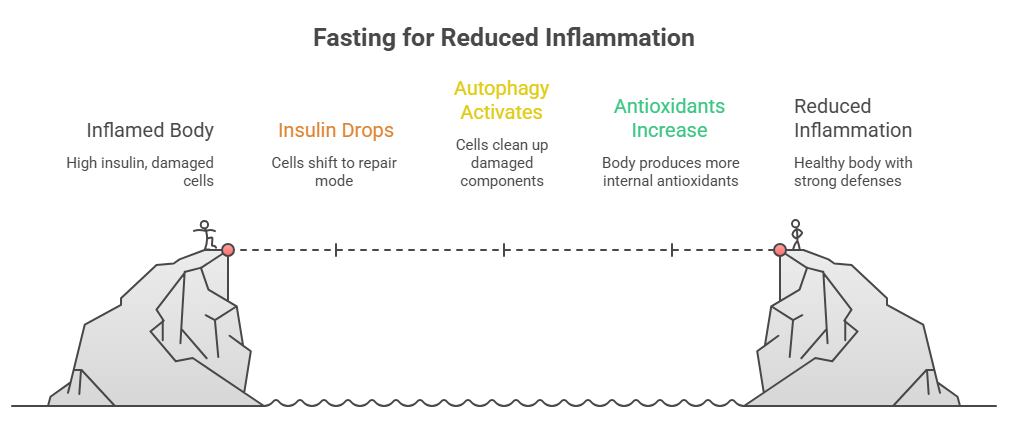
Insulin drops to baseline
Within hours of your last meal, insulin levels fall substantially. This decline reverses the inflammatory signaling that elevated insulin promotes. Cells throughout your body receive permission to shift from storage mode to repair mode.
Low insulin also allows stored fat to release into circulation for use as fuel. Your body transitions from burning incoming food to burning accumulated body fat. This metabolic flexibility was essential for survival and remains available whenever you stop eating long enough to access it.
Autophagy activates
Autophagy, which literally means self-eating, describes the process by which cells clean up damaged components and recycle them into raw materials. This cellular housekeeping removes dysfunctional proteins and organelles that would otherwise accumulate and cause problems.
Damaged cellular components contribute significantly to inflammation. Misfolded proteins trigger immune responses. Dysfunctional mitochondria leak reactive oxygen species. Autophagy clears this debris before it causes trouble, essentially taking out the cellular trash that promotes inflammation.
Autophagy ramps up substantially after 16 to 24 hours without food. Shorter fasts initiate the process while longer fasts allow more thorough cleaning. This mechanism explains why periodic extended fasts provide benefits beyond daily time-restricted eating.
Endogenous antioxidants increase
Your body produces its own antioxidant compounds that far exceed what any supplement provides. These endogenous antioxidants include glutathione, superoxide dismutase and catalase. They neutralize free radicals that drive oxidative stress and inflammation.
Fasting triggers increased production of these internal antioxidants. The mild stress of going without food activates protective pathways that strengthen your defenses. This hormetic response, where small stressors produce beneficial adaptations, explains why fasting improves resilience rather than depleting it.
Frequent eating suppresses endogenous antioxidant production. When food constantly arrives, your body sees no need to ramp up protective systems. The very act of eating so regularly prevents your internal defenses from reaching their potential.
Gut rest and repair
Your digestive tract finally gets a break during fasting. The constant work of processing food pauses, allowing repair processes to catch up. The gut lining regenerates faster when not simultaneously handling digestion.
The migrating motor complex, a sweeping wave of muscular contractions that cleans out your intestines, only activates during fasting. This housekeeping function pushes debris and bacteria toward the exit, preventing the overgrowth and misplacement that contribute to gut inflammation. Constant eating prevents these cleaning waves from ever occurring.
Research on fasting and inflammation
Scientists have documented fasting’s anti-inflammatory effects through numerous studies measuring specific biomarkers. The evidence base continues growing as researchers explore different fasting protocols.
C-reactive protein, a general marker of systemic inflammation, consistently drops in fasting studies. Reductions of 25 to 40% appear within weeks of adopting intermittent fasting practices. These improvements occur regardless of weight loss, indicating direct anti-inflammatory mechanisms beyond simple calorie reduction.
Inflammatory cytokines including IL-6, TNF-alpha and IL-1beta decrease with fasting interventions. These signaling molecules drive inflammatory cascades throughout the body. Lower levels translate to reduced inflammatory activity in joints, blood vessels, the brain and other tissues.
Oxidative stress markers also improve. Measures of lipid peroxidation and protein oxidation decline while antioxidant capacity increases. Fasting shifts the balance from damage accumulation toward repair and protection.
| Marker | Effect of Fasting | Typical Improvement |
| C-reactive protein | Decreases | 25-40% reduction |
| IL-6 | Decreases | Significant reduction |
| TNF-alpha | Decreases | Moderate reduction |
| Oxidative stress | Decreases | Improved markers |
| Antioxidant capacity | Increases | Enhanced defenses |
| Insulin | Decreases | Major reduction |
| Autophagy | Increases | Significant activation |
Human studies on conditions characterized by inflammation show promising results. Rheumatoid arthritis patients report reduced joint pain and stiffness with fasting protocols. Asthma symptoms improve in some studies. Inflammatory bowel disease patients sometimes achieve remission through carefully implemented fasting approaches.
Different fasting approaches
Several methods exist for incorporating fasting into your routine. Each offers distinct advantages depending on your goals, lifestyle and current metabolic state.
Time-restricted eating
This approach compresses all daily eating into a defined window while fasting the remaining hours. The 16:8 protocol, eating within 8 hours and fasting for 16, provides an accessible starting point. Many people naturally skip breakfast and eat between noon and 8 PM.
More aggressive windows like 18:6 or 20:4 extend fasting benefits. Some people eventually progress to one meal a day, eating within a single hour and fasting 23 hours. Greater restriction produces more pronounced effects but requires adaptation.
Time-restricted eating works well for daily practice. It requires no special planning beyond timing your meals. Social eating remains possible within your window. Most people find this approach sustainable long-term once adapted.
Alternate day fasting
This protocol alternates between regular eating days and fasting days. Some versions allow limited calories, perhaps 500, on fasting days while others involve complete abstinence from food.
Alternate day fasting produces more dramatic autophagy activation than daily time restriction. The extended fasting periods allow deeper cellular cleaning. Research shows significant inflammatory marker improvements with this approach.
The challenge lies in sustainability. Many people find true alternate day fasting difficult to maintain long-term. Modified versions allowing some food on fasting days improve adherence while preserving most benefits.
Periodic extended fasts
Fasts lasting 24 to 72 hours or longer provide the most profound metabolic effects. Autophagy peaks around day two or three of water-only fasting. Stem cell regeneration appears to activate during extended fasts, potentially explaining some of the deeper healing reported.
Extended fasting requires more preparation and monitoring than shorter protocols. Electrolyte balance becomes important beyond 24 hours. People with certain medical conditions should fast only under supervision.
Most people benefit from periodic extended fasts without making them a constant practice. A 48-hour fast once monthly or a longer fast quarterly provides autophagy and regeneration benefits while remaining practical.
Modified fasting approaches
Fasting-mimicking diets restrict calories and protein significantly while allowing some food. This approach triggers many fasting adaptations while being easier to tolerate than complete abstinence. Research on proprietary fasting-mimicking protocols shows inflammatory improvements.
Fat fasting, consuming only fat calories, maintains ketosis and low insulin while providing energy. Some people use this approach to extend fasting benefits while having something to eat. Pure fat minimally interrupts autophagy compared to protein or carbohydrates.
Getting started with intermittent fasting
Jumping straight into extended fasting rarely works well. Your metabolism needs time to adapt to accessing stored fuel. Starting gradually prevents the miserable symptoms that cause many people to quit before experiencing benefits.
Week one: delay breakfast
Simply push your first meal later each day. If you normally eat at 7 AM, try waiting until 9 AM for a few days. Then push to 10 AM, then 11 AM. This gradual approach lets your body adjust without dramatic hunger or energy crashes.
Most hunger comes from habit rather than genuine need. Your body expects food at accustomed times and generates hunger signals accordingly. After a week or two of shifted meal timing, hunger patterns reset to match your new schedule.
Week two: establish your window
Once comfortable eating later, define your eating window. Most beginners do well with 8 hours. Choose times that work with your life. Noon to 8 PM suits many schedules, but 10 AM to 6 PM or other variations work fine.
Stay consistent with your window rather than changing it daily. Consistency helps your body anticipate when food is coming and reduces hunger during fasting periods. Occasional variations won’t derail progress, but general consistency accelerates adaptation.
Week three and beyond: refine and extend
After establishing basic time-restricted eating, you can experiment with shorter windows or periodic longer fasts. Pay attention to how different approaches affect your energy, hunger and inflammatory symptoms. Personal experimentation reveals what works best for your body.
Some people thrive with longer daily fasts while others prefer occasional extended fasts with more relaxed daily eating. Neither approach is inherently superior. The best protocol is whichever one you’ll actually follow consistently.
What to consume during fasting
Water should flow freely throughout fasting periods. Adequate hydration supports detoxification and helps manage hunger. Adding a pinch of sea salt provides electrolytes without breaking your fast.
Black coffee and plain tea are generally considered acceptable during fasting. The minimal calories don’t significantly impact insulin or autophagy. Caffeine may even enhance some fasting benefits by promoting fat mobilization. Avoid adding cream, sugar or sweeteners.
Bone broth occupies a gray zone. The small amount of protein and calories technically breaks a strict fast but provides electrolytes and gut-soothing compounds. Some people use bone broth during longer fasts to improve tolerance without completely abandoning fasting benefits.
Supplements vary in their impact on fasting. Fat-soluble vitamins absorb better with food and may be better taken during eating windows. Water-soluble vitamins and minerals generally don’t disrupt fasting significantly. Fish oil contains calories that may break a strict fast but likely preserves most benefits.
Common challenges and solutions
Hunger waves
Hunger during fasting comes in waves rather than building continuously. A wave peaks and then subsides even if you don’t eat. Knowing this helps you ride out difficult moments rather than breaking your fast at the first twinge.
Staying busy distracts from hunger. Physical activity often suppresses appetite rather than increasing it during fasting. Drinking water or black coffee provides something to consume without breaking your fast.
Low energy initially
The first week or two of fasting can feel rough as your metabolism adapts. Your body has relied on constant glucose input and needs time to become efficient at mobilizing stored fuel. This transition period passes.
Ensuring adequate electrolytes helps enormously. Sodium, potassium and magnesium support energy production. Adding salt to water and eating mineral-rich foods during eating windows prevents the fatigue and headaches some experience.
Social situations
Food plays central roles in social connection. Fasting can feel isolating when everyone else eats together. Flexibility helps here. Adjusting your eating window for important social meals maintains relationships without abandoning your practice entirely.
You can also participate socially without eating. Joining friends for coffee during a fasting period keeps you connected. Many people find that explaining their fasting practice generates interesting conversations rather than awkwardness.
Maximizing fasting benefits
Fasting works best as part of a comprehensive approach rather than an isolated intervention. What you eat during feeding windows matters significantly. Combining fasting with anti-inflammatory food choices multiplies the benefits.
Breaking fasts with inflammatory foods undermines the healing you achieved while fasting. Reaching for processed foods, sugar or seed oils after an extended fast wastes the metabolic reset you worked to achieve. Plan nourishing meals to break your fasts.
Chronic stress interferes with fasting benefits by keeping cortisol elevated. High cortisol promotes inflammation through separate pathways that fasting doesn’t fully address. Understanding the connection between stress and inflammation helps you identify whether stress management needs attention alongside your fasting practice.